Paediatric Dietitians – referral criteria
Around 1 in 10 girls and 1 in 30 boys will have had a Urinary Tract Infection (UTI) by the age of 16 years
Most UTI’s can be managed in the community with oral antibiotics.
Risk factors for urinary tract infection (UTI) in children and young people include:
- Age below one year.
- Female sex — however, in the first three months of life, UTI is more common in boys than girls.
- Previous UTI
- Voiding dysfunction (eg. With neurogenic bladder, constipation)
- Vesicoureteric reflux (VUR), family history of VUR or renal disease.
- Sexual activity (NB: Sexual abuse can cause urinary symptoms, but infection is uncommon)
Definitions
UTI is best defined as the presence of a significant level of bacteria in the urinary tract causing an inflammatory response.
Lower UTI (Cystitis):
Child is usually apyrexial.
Frequency, wetting, dysuria common
Suprapubic pain
Upper UTI (Pyelonephritis):
Fever over 38oC
Loin pain/tenderness
Vomiting
Rigors
Atypical UTI :
Seriously ill
Poor urine flow
Abdominal or bladder mass
Raised creatinine
Septicaemia
Failure to respond to antibiotic treatment within 48 hours
Infection with non-Escherichia coli organism
Recurrent UTI:
2 or more episodes of upper tract UTI
1 episode of upper tract UTI plus 1 or more episode of lower tract UTI
3 or more episodes of lower tract UTI
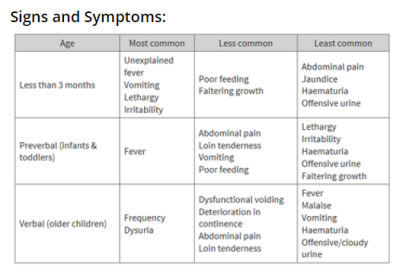
History and Examination key points:
- Ask about signs and symptoms (see table)
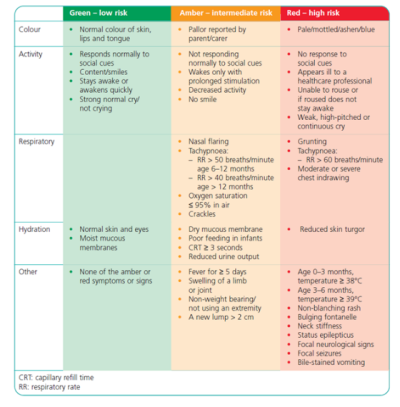
- Assess for signs of serious illness (see red flags)
- Ask about atypical and recurrent UTI symptoms
- Ask about fluid intake and history of constipation
- Ask about lifestyle/hygiene – poor wiping, washing and adequate ventilation (e.g. tight fitting clothes)
- Measure blood pressure (if possible in primary care, using an appropriate sized cuff) – if raised this could indicate underlying renal pathology
- Check for signs of a spinal lesion and abdominal masses
These include any signs and symptoms of serious illness/sepsis in Amber and Red sections below:
All children with a suspected UTI should have urine sample collected by ‘Clean catch’ – the perineal/genital area should be cleaned before collecting to reduce risk of contamination. (See supporting information for guide on this technique in young children)
Dipstick and microscopy can guide initial management. Culture results and sensitivities are then used to adjust management as appropriate.
Urine samples should be collected prior to starting antibiotics (unless the child is seriously unwell).
In children age >3 months and < 3 years: Dipstick tests are unreliable so must be sent for MC+S if any of the criteria below are met even if dipstick is negative. A sample should always be sent if leukocyte esterase and/or nitrite positive on urinalysis
- acute pyelonephritis/upper urinary tract infection is suspected
- there is a high to intermediate risk of serious illness
- recurrent UTI
- infection that does not respond to treatment within 24–48 hours, if no sample has already been sent
- when clinical symptoms and dipstick tests do not correlate.
In older children (> 3 years old) urine interpret results as below
| Dipstick |
Nitrite Positive |
Nitrite Negative |
|
Leucocyte positive |
Likely UTI – Send MC+S and start treatment |
Possible UTI – send MC+S; only start treatment if strong clinical indication |
|
Leucocytes negative |
Likely UTI – If fresh specimen send MC+S Start treatment |
Unlikely UTI |
| Age |
Treatment |
Comment |
|
<3months |
Emergency referral |
|
| >3months Lower UTI |
Trimethoprim 3 days OR Nitrofuantoin 3 days |
Assess response after 48 hrs Check culture and sensitivities |
|
>3months Upper UTI |
Well – Oral Co-amoxiclav 7-10days OR Cefalexin 7-10days Unwell/Red flags – Emergency Referral |
Assess response after 48 hours Emergency Referral if not responding/unwell |
Discuss ways to prevent further UTI’s:
- Managing constipation
- Increasing fluid intake
- Improving lifestyle/hygiene – wiping front to back and ensuring adequate ventilation using cotton fabrics.
Urgent Referrals:
Please refer to PAU (Paediatric Assessment Unit) via switchboard on 0208 546 7711 and ask to be put through to Paediatrics on call. This will be a telephone during normal working hours and the Registrar bleep out of hours. Children who sound seriously unwell may be asked to go to A&E where paediatrics can see and resuscitate as necessary.
- All children with fever < 3 months
- Children with signs of a serious infection/sepsis
- Children with signs of an atypical UTI
- Children with known renal tract anomalies
- Children with Upper UTI who are unwell/won’t tolerate oral antibiotics
Outpatient Referrals:
For outpatient referrals, please refer via ERS to general paediatrics. If you are unsure of the urgency required or would like to discuss, please contact us via Advice & Guidance on ERS in the first instance.
- Recurrent UTI – confirmed on microscopy.
NB If recurrent urinary symptoms with no confirmed UTI, please discuss preventative measures first and ensure that these have been addressed and consider vulvovaginitis as an alternative diagnosis (see separate page on Vulvovaginitis)
- Atypical UTI
- Dysfunctional voiding
- Suspected underlying renal cause for symptoms
- Evidence of spinal lesion
https://
https://
https://
https://
Urinary tract infection in children
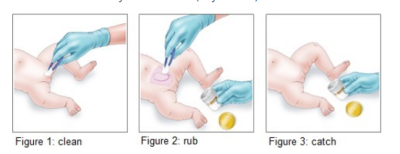
Clean catch Urine Collection:
The following is useful information for parents on how to catch a urine sample:
This method involves trying to catch some urine in a sample container that your doctor will give you. Start by offering your child a drink (cup, bottle, breastfeed). Most children who are going to wee for a clean-catch will do so within one hour.
- Have the sample container ready.
- Remove your child’s nappy.
- Wash your hands thoroughly before collecting the sample, or wear gloves.
- Clean the skin around the genital area. Use clean plastic tweezers and gauze soaked in water if available, or use baby wipes (Figure 1).
- Keep watching until your child does a wee. Be ready to catch a urine sample in the container when the wee comes.
- To encourage your child to wee, you can gently rub their lower abdomen (tummy) for a few minutes using a clean piece of gauze soaked in cold water (Figure 2).
- Hold the container away from your child’s skin when catching the urine (Figure 3). This is important so that bacteria from your child’s skin (or your skin) don’t contaminate the urine sample.