Paediatric Dietitians – referral criteria
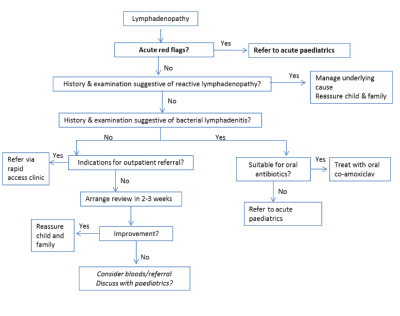
Lymphadenopathy (or ‘swollen glands’) is very common in children. In fact, it is estimated that around 50% of otherwise healthy children may have lymphadenopathy at any one time.In the majority of children, lymphadenopathy is usually reactive. This is a normal response to childhood infections such as colds or tonsillitis. It is also seen in children with eczema or babies with cradle cap.Localised swelling or fever may indicate bacterial lymphadenitis requiring antibiotics. Rarely, lymphadenopathy may form part of presentation of less common infections or haematological malignancy.Lymphadenopathy refers to lymph nodes abnormal in size, consistency or number. Lymph nodes greater than 1.5cm in diameter in the groin, or 1cm anywhere else, are defined as raised. However, in practice, cervical lymph nodes less than 2cm in diameter are unlikely to indicate severe pathology.

The following are considered ‘Red Flags’ for significant pathology and would warrant paediatric referral.
• Severe pallor
• Weight loss
• Loss of appetite
• Loss of energy
• Fever/signs of sepsis
• Unexplained bruising or bleeding
• Any suggestion of mediastinal mass (shortness of breath or discomfort lying down, unexplained fever or night sweats, unexplained weight loss, chest pain)
Most children with simple lymphadenopathy need no further investigations. See under management for those who might.
Most enlarged lymph nodes require no management or further referral unless there are any red flags.
In cases of reactive lymphadenopathy, please reassure the child and family that this is a normal response to infection. Lymph nodes are likely to slowly decrease over time, though this may take 2-4 weeks. It is normal for the lymph nodes to get bigger and smaller in future with intercurrent infections.
Suspect bacterial lymphadenitis if there is a short history of infection and lymph node is red and/or tender. If the child is well, consider treating with co-amoxiclav orally. If no response to oral antibiotics, systemic illness, fluctuant mass or more than 5cm then refer to acute paediatrics on-call for consideration of admission for IV (intravenous) antibiotics.
If there are any acute concerns as listed above, then refer in to acute paediatrics via the GP referral phone. The child is very likely to need further investigations including a blood test.
The following would be indications for referral to rapid access clinic (which is currently accessed by ERS and marked as ‘urgent’)
• Cervical lymphadenopathy more than 2cm in diameter and increasing in size or present for more than 2 weeks
• Unexplained inguinal lymphadenopathy more than 1.5cm in diameter
• Unexplained axillary, epitrochlear or supraclavicular lymph nodes of more than 1cm diameterIf possible, please arrange FBC, blood film, LFTs, ESR, consider Monospot (if aged > 5 years and clinical suspicion of acute EBV), consider ASOT/CMV/EBV serology if thought to be relevant.
For cases where there is clinical uncertainty or you would like to discuss the patient, please contact paediatrics via Kinesis. For urgent queries, please call switchboard, and ask to speak to the on call Paediatrics Team via the PAU Telephone.