Paediatric Dietitians – referral criteria
Head Injury is a common presentation to A+E in all ages. Causes include falls, play/sporting accidents, road traffic accidents and non‐accidental injury. In the UK, trauma is classified as the most common cause of mortality and morbidity in children over 1 year.However, most head injuries which are caused by low impact mechanisms are not serious. Children do not usually have to attend hospital and will recover within 2 weeks. The presence of red flag symptoms is an indicator of significant trauma or resultant raised intracranial pressure.All children under 1 year of age, or those who are non-ambulant, should be seen and assessed in hospital following a head injury. In this age group, who are difficult to assess clinically, head injuries are more likely to be significant or caused by non-accidental injury (NAI).
History• What is the mechanism? What height/speed did it occur at?• When did it occur?• Loss of consciousness? For how long? Any seizures/abnormal behaviour?• Has there been any vomiting? If so how many EPISODES (children often vomit once or twice after a head injury. Two vomits in quick succession would count as one episode.)• Does the child have a Headache or signs consistent with a headache?• Any altered behaviour?• What has been the clinical course prior to consultation – improving/stable/deterioration• Any other injuries? Important to consider cervical spine injuries.• Is the child on any anti-coagulants?• Any concerns as to how the injury occurred? Unattended child? Possible non-accidental?
Examples of High Energy Head Injuries• High speed/rollover motor vehicle collision• Child struck by motor vehicle or ejected from motor vehicle• Fall from height greater than 1 metre (or more than 5 stairs)• Most Bicycle collisions• Fall from/ trampled by a large animal• Impact from golf club, cricket or baseball bat
Non-Accidental InjuryAlways consider Non accidental Injury (NAI), especially if the mechanism of injury does not fit the injury or the child’s age. If you think NAI is a possibility, please arrange urgent paediatric review by calling the PAU phone (via switchboard). It is impossible to assess the likelihood of a high impact injury if you cannot rely on parental/carer account.
Please refer urgently and send the child to Children’s A&E if there are any of the following red flags and the child will be assessed for consideration of performing a CT head (as per NICE guidelines).
The following table of ‘red flags’ are signs which may necessitate a CT scan of the head. Any child with a ‘red flag’ should be urgently transferred to the nearest Emergency Department. Please use clinical judgement to decide whether a ‘999’ paramedic is required.
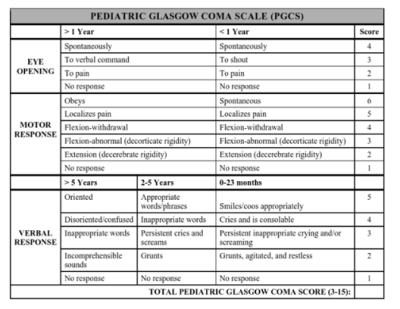
Red Flags• On initial assessment, GCS less than 14, or for children under 1 year GCS (paediatric) less than 15.• At 2 hours after the injury, GCS less than 15.• Suspected open or depressed skull fracture or tense fontanelle.• Any sign of basal skull fracture – haemotympanum, ‘panda’ eyes, cerebrospinal fluid leakage from the ear or nose, Battle’s sign.• Focal neurological deficit.• Post-traumatic seizure but no history of epilepsy.• For children under 1 year, presence of bruise, swelling or laceration of more than 5 cm on the head.• Suspicion of non-accidental injury• Loss of consciousness lasting more than 5 minutes (witnessed).• Abnormal drowsiness.• Three or more discrete episodes of vomiting.• Dangerous mechanism of injury (high-speed road traffic accident either as pedestrian, cyclist or vehicle occupant, fall from a height of greater than 3 metres, high-speed injury from a projectile or other object).• Amnesia (antegrade or retrograde) lasting more than 5 minutes.
As above, if there are any ‘red flags’ present, please refer urgently to hospital. This is best via Paediatric ED.If the head injury is minor, has no red flags (including no safeguarding concerns), and the examination is reassuring, the following is advice for parents observing their child at home. This should be explained carefully to parents before sending home. This should also be backed up with written advice as per NICE – their suggested written advice is here (advice for < 16 years is at the end)https://
Post Head Injury Advice for Parents:• Do not leave them alone in the first 24hrs• It is OK to allow your child to sleep, but observe them regularly and check that they respond to touch and that both their breathing and position in bed is normal• Observe your child closely for the next two to three days and check that they are responding to you as usual• Make sure they have plenty of rest and avoid stressful situations• Check that they can respond to you normally and can move their arms and legs normally• Give your child Children’s liquid paracetamol or ibuprofen if they are in pain. Always follow the manufacturers’ instructions for the correct dose.• If the area is swollen or bruised, try placing a cold facecloth over it for 20 minutes every 3-4 hours.• Make sure they are completely recovered before allowing them back to school• Do not allow them to play contact sport for three weeks without speaking to your GP
If there is a related injury that needs assessment eg: laceration or limb injury, please consider whether this needs A&E, or minor injury unit assessment.
The following table is a guide for parents as to where they should go if their child has sustained a head injury:
Has the child:
Been knocked out at any time?Injured their neck or spine?Had difficulty understanding what the parent/carer is saying?Been confused or so sleepy that the parent/carer cannot wake them properly?Complained of tingling or numbness (lack of feeling in arms or legs)/shown any weakness in their arms and legs?Have they been clumsier than usual – having problems with their balance?Had a fit or convulsion since the head injury?Become suddenly deaf?Had clear fluid dribbling out of their nose, ears or both?Had blood coming from inside one or both ears? more than once? Bled a lot from their head? If YES to any of the above phone 999 for an ambulance to take the child to A&E.
Has the child:
Fallen from a height greater than their own height? (eg. a baby rolling off a bed)Fallen more than a metre in height?Fallen down stairs? Was it from top to bottom or did they bump down the stairs? (bumping down poses less risk)Had a persistent headache since the injury?Had a blood clotting disorder?Consumed alcohol?Been very irritable or “not themselves”, no concentration or interest in things around them?Are you concerned that your child may have been deliberately abused? If YES to any of the above consider taking the child to A+E or obtaining medical advice
If the child:
Has not been “knocked out”?Is alert and interacts with the parent? Has been sick but only once?Has bruising or minor cuts to their head?Cried immediately but is otherwise normal?-> Give self-management advice. Advise them to contact their GP, NHS Direct or go to the Walk–in–Centre if they have any concerns.
For more detailed information please see:– NICE Head injury Guideline: https://
Has bruising or minor cuts to their head? Cried immediately but is otherwise normal? -> Give self-management advice. Advise them to contact their GP, NHS Direct or go to the Walk–in–Centre if they have any concerns.